It is a tissue growth caused by the continued proliferation of abnormal cells with invasiveness and destruction of other tissues.
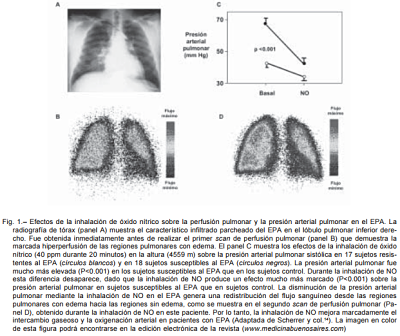
The cancer, which may originate from any type of cell in any body tissue, it is not a single disease but a group of diseases that are classified according to the tissue and cell of origin. There are several hundred different ways, with three major subtypes: the
sarcomas come from connective tissue such as bone, cartilage, nerves, blood vessels, muscles and adipose tissue. Carcinomas originate from epithelial tissues such as skin or the epithelial cells lining the body cavities and organs, and glandular tissue of the breast and prostate. Carcinomas include some of the most common cancers. Carcinomas skin - like structure called squamous cell carcinomas. Those with a glandular structure are called
adenocarcinomas . In the third subtype are leukemias and lymphomas, including cancers forming tissue blood cells. Cause inflammation of lymph nodes, invasion of the spleen and bone marrow and overproduction of immature white cells.
Carcinogenesis
Inheritance : It is estimated that 5 to 10% have a hereditary cancers origin. Some forms of cancer are more common in some families , the breast cancer is an example. The colon cancer is more common in families with a tendency to colon polyps. A form of retinoblastoma appears only when a specific gene is absent. These genes, called tumor suppressor genes or anti - oncogenes, normally prevent cell replication. His absence removes normal control of cell multiplication. In some inherited disorders, chromosomes have an intrinsic fragility; These processes involve a high risk of cancer.
Chemicals : Coal tar and its derivatives are considered highly carcinogenic. Its vapors in some industries (eg. Refineries) are associated with the high incidence of lung cancer among workers.
Today it is known that benzopyrene, chemical present in coal, causes the skin in people whose jobs are related to coal combustion cancer.
Arsenic is associated with lung cancer , as workers of copper and cobalt mines, smelters and factories insecticides have an incidence of this type of cancer higher than normal. Workers in asbestos - related industries, the incidence is up to 10 times more than normal.
A substance produced by the fungus Aspergillus flavus, called aflatoxin, and contaminates poorly preserved foods, causes liver cancer in some animals. It has been found that in countries where food contamination by molds is common, the incidence of liver cancer and stomach is high.
Smoking is another carcinogen, it has been determined that death from lung cancer is 6 times higher among smokers than non-smokers between. The cigarette is so pernicious because the substances contained therein; nicotine, acids and carbon oxides and tar.
Alcohol is also a major promoter; its chronic abuse significantly increases the risk of cancers that are induced by other agents.
Radiation : Ionizing radiation is one of the most recognized causal factors. The radiation produces changes in DNA, such as chromosomal breakage or transpositions where the broken ends of two chromosomes can be interchanged. Radiation acts as an initiator of carcinogenesis, inducing alterations progressing to cancer after a latency period of several years. The sun 's ultraviolet rays and X - rays increase the propensity to acquire skin cancer and leukemia. Excessive exposure to sunlight, by people with white skin, increases the risk.
Infections or viruses : There is increasing evidence that some infections can even cause cancer and in particular those related to cancers of the stomach, liver, cervix and the Kaposi's sarcoma (a special type of cancer that occurs in patients AIDS). It has been associated with Helicobacter pylori stomach cancer. Several studies show that people infected with this bacterium are four times more likely to develop this cancer.
Viruses are the cause of many cancers in animals. In humans, the Epstein-Barr virus is associated with Burkitt's lymphoma and lymphoepitheliomas, the hepatitis with liver cancer, and herpes virus type II or genital herpes virus with cervical carcinoma. All of these viruses are human tumor - associated DNA type. HTLV virus, however, is the RNA type, or retroviruses, as most of the associated viruses tumors in animals. It produces a human leukemia. In the presence of an enzyme called reverse transcriptase, induce the infected cell to produce DNA copies of the virus genes, which in this way are incorporated into the cell genome. These RNA virus containing a gene called viral oncogene capable of transforming normal cells into malignant cells. Research has shown that viral oncogenes have a counterpart in normal human cells: the proto - oncogene, or cellular oncogene. The products of oncogenes (the proteins they produce) are growth factors (or proteins necessary for the action of such growth factors) that stimulate the growth of tumor cells.
Traumas : mechanical irritation produced on a portion of the skin and friction exerted on moles is considered harmful. Lip cancer in pipe smokers is associated with chronic irritation from the pipe on a group of cells on the lip. In India, a high incidence of cancer of the abdomen and groin relates to clothing (a sort of loincloth) in widespread use.
epidemiology :
Frequency : Cancer is the second leading cause of death. Cancer deaths are increasing. It is estimated that over the twenty - first century cancer will be the leading cause of death in developed countries. Despite this, there has been an increase in the median survival of patients diagnosed with cancer.
Type: the relative frequency of each type of cancer varies by sex and geographic region. The lung cancer is the most common in the world for total both sexes especially in men, whereas in women is breast cancer . In the United States, excluding skin cancer, the most common in men are lung, prostate and colorectal cancers, while in women the first is lung cancer, followed by breast cancer and colorectal cancer. In Europe, in men, prostate cancer is the most common, followed by lung cancer and colon and rectum. In women, the most common is breast cancer, followed by colorectal and lung cancer.
For new cases of cancer diagnosed in a population over a period of time, called population cancer registries are used, which are concerned with collecting systematically, continuously and standardized information necessary for cancer incidence data and study their distribution by age, sex, tumor characteristics and its evolution over time.
Clinical manifestations of malignant neoplasms : Between 5 and 10% of patients with lung cancer have no symptoms at presentation of the disease and only be seen on chest radiographs, while the remaining percentage will present at least one symptom of the time of diagnosis.
In lung cancer has signs and symptoms because of :
- Growth in a particular region of the tumor.
- Obstruction of nearby or adjacent structures.
- The growth of regional lymph lymphatic decline.
- Growth in distant metastatic sites after hematogenous dissemination and remote effects of products synthesized by the tumor.
Most cancers present an intense cough is the most common symptom and is usually the earliest. It may be dry but often is accompanied by a mucupurulenta expectoration. The hemoptysis or hemoptysis is less frequent, usually a late but very significant sign.
Metastatic carcinomas prefer the interstitial tissue and cause few symptoms if not obstructing a bronchus.
Pain is another common symptom, you can be felt in the shoulder, arm, chest wall or even in the epigastrium. It depends on the location of the tumor and whether Cervicobrachial affecting the plexus, intercostal nerves, periosteum or cause atelectasis or pleurisy. The ipsilateral contorsion is a late sign.
1. SYMPTOMS RELATED TO LOCAL TUMOR GROWTH ARE :
Central location: may have cough, shortness of breath, recurrent pulmonary infections, hemoptysis.
Peripheral location: chest pain, dyspnea, pleural effusion, necrosis, cavitation and subsequent formation of lung abscesses.
2. Symptoms related to primary lesion :
Tos : The most common presentation of lung cancer (74%), relative to endoluminal tumor growth. If cough appears with intake has been suspected in tracheoesophageal fistula may appear boxes mucopurulenta side coughing up the bronchial tumor growth level producing the clinical picture called obstructive pneumonitis. For the endobronchial tumor growth itself can cause stridor, necrosis and consequently bleeding.
Dyspnea: It occurs in 60% of patients, usually associated with an increased cough and sputum , can translate airway involvement, pericardial effusion pericardial involvement, obstructive pneumonitis, carcinomatous lymphangitis or pulmonary embolism.
3. SIGNS AND SYMPTOMS OF SPREAD CHEST :
Intrathoracic spread of lung cancer, either by direct extension or lymphatic spread, produces a variety of signs and symptoms. These may be caused by the engagement of the following structures:
- As the recurrent laryngeal nerves, phrenic, brachial plexus, and nerves of the sympathetic trunk.
- Pleura and chest wall.
- Vascular Commitment as the superior vena cava, pericardium and heart.
- Organs including the esophagus.
Recurrent laryngeal nerve paralysis: it has been reported in 18% of cases and is more common in tumors located in the left side of the chest wall, causing hoarseness, and is associated with increased risk of aspiration.
Phrenic nerve palsy: radiologically demonstrated by the elevation of hemidiaphragm.
Chest pain: by engagement of the wall is a common symptom; more than 50% of patients report chest pain during the course of the disease, it is usually dull poorly localized, persistent, and not related to respiration or cough. The sternal retro pain can make us suspect a massive mediastinal and hilar lymph node involvement. If it may be located direct invasion of the pleura or metastasis ribs.
The pleura is involved in 8-15% of cases, presenting pleuritic pain that occurs early, phased out with the introduction of pleural effusion.
Invasion of heart and pericardium: The heart and pericardium are involved by direct lymphatic spread, and occurs in 15% of cases, occurring as a result in rare cases cardiac tamponade.
Esophageal invasion: Esophageal compression occurs most often by the presence of Subcarinal posterior mediastinal lymph node invasion and no symptoms unless your commitment is massive and usually this translates to dysphagia.
ANAMNESIS
The doctor performing medical history, collect information from:
- History of disease like chronic bronchitis, emphysema, asbestosis, tuberculosis.
- Occupation.
- Harmful habits.
- Symptoms presented by the patient.
- Presence of dominant or recessive oncogenes.
A detailed medical history and a good physical examination can suspect the diagnosis of a tumor. Thus, an important and with a family history of lung cancer patients who smoke oriented toward malignancy. The presence of recurrent respiratory infections, as well as increased cough with hemoptysis are suggestive of pulmonary neoplasm.
- The occurrence of hoarseness guides the involvement of the recurrent laryngeal nerve .
- The facial edema and dyspnea they suspect the diagnosis of superior vena cava syndrome.
- Bone pain suggestive of bone metastases.
- Neurological brain pictures aimed at dissemination.
1. PHYSICAL EXAM:
A physical examination will be performed to assess the overall situation of the patient, paying particular attention to the signs that may express an extension to the rest of the chest or other body organs.
TO). INSPECTION:
- Observe the symmetry of the posterior thorax, position and mobility during respiration.
- Visual inspection of the thorax in its front, back and sides allow you to appreciate: thoracic deformation can be localized inflammatory or neoplastic origin.
- Presence of nodules or lumps.
B). PALPATION:
- Reduction or abolition of vocal vibrations.
- A previous neck palpation should seek lymphadenopathy secondary to mediastinal lymph commitment by neoplasms.
- Presence of painful points.
C). PERCUSSION:
- Dullness according to the tumor site.
D). AUSCULTATION
- Reduction or abolition of breath sounds.
- Presence of wheeze.
WHO classification:
1. Squamous cell carcinoma or squamous cell :
Usually presents the central location, near a main airway (bronchus). Although 20% are peripheral, 80% of squamous cell carcinomas have an endobronchial component , and its tendency to delamination, can be detected by sputum cytology. The frequency is 35% of all lung cancers, currently its biggest relation to snuff, is in decline, ranking second after adenocarcinoma.
Histologically, they are characterized by intercellular bridges existence of desmosomes, squamous cell formation and keratinization pearlescent single large pleomorphic cells, abundant cytoplasm, prominent nucleoli. Given its growth at the level of the segmental bronchi, prone to the invasion of lobar is frequent occurrence of obstructive pneumonitis.
In the macroscopic, most of these tumors are large and develop central necrosis, forming caverns , and are presented as a yellowish gray mass of firm consistency with congestive vessels, areas of hemorrhage and necrosis; usually they reach large sizes before metastasize, related to smoking and is more common in men.
2. Adenocarcinoma (including bronchoalveolar):
They are the most common histological types of lung cancer, accounting for 46% of cases. Predominates in women and nonsmokers.
It comes from the distal epithelia and mucous glands, which tends to be in their peripheral location, reaching no more segmental bronchi and bronchioles. They may appear as solitary pulmonary nodules in chest standard. These tumors tend to spread hematologically, and linfáticamente.
Histologically usually has a good glandular differentiation, with formation of acinar structures and produce mucin secretion . It has been associated with previous lung scarring areas. Histological subtype called bronchoalveolar which grows from the alveoli so it is believed originates from type II pneumocytes, forming columnar structures along with important alveoli differs mucin production. It may present as a solitary pulmonary nodule, with multifocal disease or rapidly progressive pneumonia.
Clinical findings do not differ from a constitutional syndrome with fever, fatigue, weakness, however, given their tumor component has a higher incidence of thrombotic complications, than other types of tumor.
Large cell carcinoma
It comes with a frequency of 10% - 13%. There are 2 variants, one of large cells and other clear cell .
They have large cells with abundant cytoplasm, large nucleus and prominent nucleoli. They can occur as peripheral tumors, with frequent areas of necrosis. They are poorly undifferentiated tumors.
Are undifferentiated malignant epithelial tumors lacking histologic features of small cell carcinoma and glandular or squamous differentiation. Typically, cells have large nuclei, prominent nucleoli and moderate cytoplasm. Large cell carcinomas or adenocarcinomas probably represent squamous cell carcinomas that are so undifferentiated that can no longer be recognized by optical microscopy.
Carcinomas small cell lung (WACC) appear as masses central location of pale gray, with extension into the lung parenchyma, and early involvement of the hilar and mediastinal lymph. these cancers are formed by tumor cells round to fusiform, scant cytoplasm and finely granular chromatin. Mitotic figures are frequently observed.
It gives early metastasis. It is associated with smoking. It metastasizes early and poor prognosis.
Imaging: The image is large and usually peripheral. Imaginological has similar characteristics with adenocarcinoma, except for its size, generally greater than 4.0 cm.
small cell carcinoma (oat cell)
It represents about 15% of all bronchial carcinomas and 20% of all positive biopsies. Predominantly affects males in ratio of 19: 1. At diagnosis more than 80% have extrathoracic extension. Despite the name of small, the size of the neoplastic cells typically twice larger than resting lymphocytes. Invariably there necrosis, which can be extensive. tumor cells are very fragile and often show fragmentation and "crushing device" in small biopsy samples. Another feature of the cell carcinomas, best seen in cytological samples, is the nuclear molding the narrow position of the tumor cells with scant cytoplasm. various neuroendocrine tumors express these markers in addition to secrete many polypeptide hormones that can produce paraneoplastic syndromes.
It is usually located in major or lobar bronchi. Invade bronchi and causes hilar masses and / or perihilar of significant size. It is associated with extensive metastatic nodal involvement hilar and mediastinal.
Distance Da early metastasis. Very poor prognosis. Associated with smoking.
Lung cancers spread in four main ways: 1. Local Propagation tumors spread locally to the surrounding lung, peribronchial spread to distant parts of the lung is frequent, direct extension to the pleura and adjacent mediastinal structures is characteristic of advanced disease.
2. lymphatic spread: The ipsilateral and contralateral to the spread peribronchial and hilar lymph nodes can cause symptoms by compressing adjacent structures.
3. Transcoelomic Propagation: Tumor cells can plant within the pleural cavity, causing a malignant pleural effusion.
4. hematogenous spread: The main sites are spread by blood the brain, bone, liver and adrenal structures.
METASTASIS:
Extrathoracic: The most common sites of metastases are the bones in 5% of the cases liver, adrenal glands, lymphatic chains intra - abdominal, brain, spinal cord, and skin.
Bone metastases: Pain resulting from bone metastases is seen in about 0 to 5% of cases as initial diagnosis. The most common sites are ribs, spine, pelvis, femur and are lytic lesions.
Liver metastases: Liver metastases rarely cause changes in laboratory data until they are many, are presented with weakness and weight loss and reveal a poor prognosis.
Adrenal gland metastases: At diagnosis, 5 - 10% of patients with non - small cell carcinoma have metastasis adrenal glands. Most metastases to the adrenal gland is located on the same side of the primary tumor , indicating that occurs by lymphatic route , while when we found contralateral to the tumor, it is considered an initial manifestation of a spread via the blood .
Metastasis in the central nervous system: Lung cancer is the primary site of approximately 70% of all cancers have symptomatic brain metastases.
CLINICAL PICTURES FOR LUNG CANCER:
paraneoplastic SYNDROME
In patients with a neoplasm, it is relatively common the appearance of a paraneoplastic syndrome (SP), in some cases, may be the first symptom. Among malignant tumors, it is most often seen in lung cancer; This fact is important to consider, especially in the presence of a neurological or endocrine SP that can facilitate earlier diagnosis and, in some cases, more effective treatment of the underlying disease.
The evolution of the SP is usually parallel to the underlying tumor, however, its management requires not only control the tumor, but also adopt specific therapeutic measures, since the evolution of the SP, as occurs in malignant hypercalcemia, you can threaten the patient's life.
Neurologic paraneoplastic syndromes
The Ca ++ lung is accompanied in 10-15% of cases of any neurological complication, usually metastatic origin. The SP occurs in approximately 1% of patients with a malignant tumor, is more common in the Ca ++ bronchogenic and the small cell histologic type usually associated with these paraneoplastic disorders, such as the S. myasthenic Eaton-Lambert (SMEL) , limbic encephalitis and subacute sensory neuropathy (NSS), it occurs in approximately 3% of patients.
ENDOCRINE paraneoplastic syndromes
It is known the ability of some non-endocrine tumors, bronchogenic specially Calcium, to produce and release small amounts of hormones or hormone precursors leading to a SP.
Among the lung or any other organ malignancies, the SP are more common in small cell Calcio. Are observed at a rate of 12%, although this figure varies, depending on the degree of judgment or study is required, from purely clinical to purely analytical (subclinical).
Some of the most common paraneoplastic syndromes in lung cancer:
systemic:
- Anorexia, cachexia, weight loss.
- Fever.
- Polymyositis, dermatomyositis.
- Orthostatic hypotension.
- Nonbacterial thrombotic endocarditis.
- Systemic lupus erythematosus.
Endrocrinos or metabolic:
- S. Cushing.
- Gynecomastia.
- Galactorrea.
- Hypertension.
- Acromegaly
- Hyperthyroidism.
- Hipercalcitoninemia
- S. carcinoid.
- Hypercalcemia.
- Hyponatremia.
- Hyperglycemia, hypoglycemia.
- Hypophosphatemia.
- Lactic Acidosis.
- Hypouricemia.
- Hyperamylasemia.
cutaneous:
- Clubbing, hypertrophic osteoarthropathy néumica.
- Acanthosis nigricans.
- Diffuse hyperpigmentation
- Erythema giratum
- Erythema multiforme.
- Itching, urticaria.
- Tylosis
hematologic:
- Anemia, polycythemia.
- Coagulopathy.
- Thrombocytopenic purpura.
- Dysproteinemia (including amyloidosis).
- Leukocytosis, Leukoerythroblastic reaction.
- Eosinophilia.
Neurological:
- Union neuromuscular and muscle.
- S. Eaton-Lambert
- Myasthenia gravis
- Polymyositis
- Dermatomyositis
- Peripheral nervous system
- Autonomic Neuropathy
- S. Ogilvie
- Sensorimotor neuropathy
- Motor Neuropathy Subacute
- Subacute sensory neuropathy
- Central Nervous System
- Dementia
- Encephalomyelitis
- Cerebral Encephalitis
- Limbic Encephalitis
- Myoclonus-opsoclonus
- Optic neuritis and retinopathy associated with cancer
- Subacute cerebellar degeneration
- Subacute necrotizing myelopathy
Renal:
- Glomerulonephritis.
- S. nephrotic.
SYNDROME Superior Vena Cava
The superior vena cava syndrome (SVCS) is the set of symptoms and signs resulting from the partial or complete blockage of blood flow through the superior vena cava to the right atrium. It may be due to intrinsic thrombosis (idiopathic or primary) or extrinsic compression (with or without secondary thrombosis).
It is one of the few medical emergencies in oncology, so early diagnosis is key to effective treatment and a better prognosis in the medium term.
In our environment malignant diseases are the most common cause of SVCS. Tumors are the most common lung cancers, accounting for 70% of all cases of SVCS, especially small cell and lymphomas. There are some benign causes of SVCS that are quite rare.
The most frequent and early symptom is breathlessness. Patients can also refer cough, hemoptysis, chest pain, dizziness and vision disorders . Clinical examination is characterized by the classic triad of: edema tippet (face, neck and both supraclavicular regions, sometimes, if the SVCS is highly evolved may also be edema in the right arm), cyanosis face and upper extremities and circulation thoraco-brachial collateral. It is customary, the finding of engorgement of the jugular veins.
This set of symptoms and signs resulting from the partial or complete obstruction of the superior vena cava. It is produced by the compressive effect of tumor masses either of lung, mediastinal lymphadenopathy or thymic origin. The most common case is bronchogenic carcinoma.
Malignant diseases are the main cause, the most common lung cancer.
Symptoms and signs
Dyspnea is the earliest symptom, subsequently accompanied by edema and swelling facial and arm level.
Cough, dyspnea, chest pain, Dysphagia, cyanosis, congestion, headache, dizziness.
Triad:
1.Circulación toracobraquial collateral.
2.Edema in tippet.
Facial 3.Cianosis
Etiology
The most common cause of superior vena cava syndrome are neoplasms, such as: the lung cancer including small cell lung carcinoma non small cell , Burkitt's lymphoma, lymphoblastic lymphoma, pre-lineage T - cell leukemia acute lymphoblastic (rare), acute leukemias and others. It can also occur as a result of thrombosis in the superior vena cava, although this is less common (about 35% due to the use of intravascular devices).
Treatment
Treatment may be medical, surgical, in this case, go directly to search for the underlying cause, and according to it, choose the most appropriate therapeutic approach. Glucocorticoids (such as prednisone or methylprednisolone) decreases the inflammatory response to tumor invasion and edema surrounding the tumor. In addition, diuretics are used to reduce venous return to the heart, which relieves pressure increase, the latter option is useful independent of the underlying cause of occlusion of the superior vena cava.
The treatment has to be established as soon as possible and be based on two fundamental aspects: initial symptomatic relief and treatment of primary malignant process.
Diagnosis
The suspected diagnosis is extremely important, because it will depend on the long-term prognosis of the patient when the neoplastic disease debut as a SVCS.
For diagnostic imaging techniques are used such as chest radiography, chest scan (CT), sometimes bilateral axillary and magnetic resonance venography. Histological diagnosis is critical to recommend a specific treatment.
Forecast
In the case of secondary to neoplasia, symptoms are relieved with radiation therapy within one month of treatment. However, even with treatment, 90% of patients die within two and a half years.
Horner's syndrome
The syndrome Claude Bernard Horner is due to a disorder or injury of the sympathetic nervous system of the face. The Claude Bernard Horner syndrome is secondary to injury of a sympathetic nerve in the neck. It manifests for 5 precise signs:
- A lowering of the upper eyelid or ptosis
- A reduction in the volume of contracted pupils or pupil or miosis
- A collapse of the eye in the orbit or enophthalmos
conjunctival injection (red eye).
- An absence of sweating in the neck and face level called anhidrosis (facial dryness).
Causes
Rarely, Horner syndrome is congenital (birth). Usually the syndrome is due to a previous injury or illness.
The most common causes are usually:
- Spinal cord injury
- Injury of the carotid artery (thrombosis, aneurysm, ...)
- Diseases or tumors involving the lung apex (top of the lungs)
- Epidural Anesthesia
- Anatomy
The sympathetic pathway is compromised in this syndrome has three neuronal levels:
1. Central level or first order neuron. From the hypothalamus, brainstem through until the cervical-thoracic spinal cord (C7-T2).
2. preganglionic level or second-order neuron. From the spinal cord, crosses the chest cavity from the top, with important anatomic relationships with Vertex Pulmonary and the subclavian artery, and ascends the neck to the top, up to the angle of the jaw cervical ganglion.
3. postganglionic neuron or third order. From the superior cervical ganglion, it gives rise to the neural pathways of the eye and face separately.
In general, clinical findings will vary depending on the level of injury.
PHYSIOPATHOLOGY
There are many potential causes of Horner syndrome, for example, disruption or dysfunction of sympathetic nerve fibers in any of the layers described above, including hypothalamic and spinal cord. This alteration may be due to varied injuries, ranging from a stroke in the hypothalamus, in brainstem syndrome (Wallenberg), or injury in the carotid artery until tumors in the upper lobe of the lung or upper pleura (tumors Pancoast), and cluster headaches.
Patients with cervical spondylosis may not exhibit symptoms of the disease itself, except for CBH and slight neck pain.
Lyme disease can cause CBH center or second neuron, reversibly.
Tumors of the nasopharynx (nasopharynx) large, affecting the skull base can cause this syndrome by compression of the sympathetic pathway.
Pancoast tumor, located at the apex of the lung produces compression syndrome chain ganglia or sympathetic efferent pathway.
In rare cases, Horner syndrome may be congenital (present at birth) and be associated with lack of pigmentation of the iris. Ear drops and certain medications can also lead to this condition is present.
Clinic
In addition to the signs and symptoms of the underlying cause, are the signs and symptoms of CBH, which are:
Ptosis : Fall of the upper eyelid unilaterally and incomplete, which added to the elevation that occurs in the lower eyelid conditions the false impression enophthalmos.
Miosis: It is a contraction of the pupil produced by paralysis of the iris dilator muscle. Generally not marked, the difference being the size of the smaller contralateral pupil of 1 mm. Increases in the dark, and varies according to the basal size of the pupil, the alertness of the patient, the degree of accommodation of the lens. Importantly anisocoria physiological (normal) is 10% of the population, with a difference in size between 0.4-0.6 mm both pupils.
Anhidrosis: O loss of sweating only occurs in patients with central or preganglionic CBH.
Delayed expansion: Normally the pupil dilates completely after five seconds of retired the luminous stimulus. In CBH, this period is increased to 15-20 seconds on the affected side, being the normal contralateral side. It is a specific sign of CBH, but is not always present.
Heterocromía: It is common to see alteration of the pigmentation of the iris of the affected in congenital CBH side, but not constantly. Rarely there is progressive heterocromía in the acquiree CBH.
In acute and due to loss of the affected side vasomotor control manner, temperature rise, with unilateral facial erythema, conjunctival hyperemia, lacrimation and nasal secretion. Subsequently, by developing hypersensitivity sympathetic vasoconstriction it occurs with decreasing temperature on the affected side, pallor and decreased sweating.
Lab
It is necessary to conduct a thorough neurological examination in order to establish the diagnosis and determine if any other part of the nervous system is affected, in order to define the cause. Some of the tests may include:
- MRI of the head
- Carotid Ultrasound
- Chest x-ray
- CT chest
- Blood tests
- Angiogram
- Ophthalmological and / or examination neuroftalmológico.
Treatment
Treatment depends on the underlying cause. There is no specific treatment for Horner syndrome itself.
Forecast
Prognosis depends on the success you have with the treatment of the underlying cause.
Pancoast tumor
Pancoast syndrome, Pancoast tumor , of Ricaldoni syndrome, tumor apex or syndrome apico-cost-vertebral is a set of signs and symptoms characteristic caused by the involvement of the nerve roots eighth cervical and first two thoracic roots and / or cervical sympathetic system by the presence of a tumor in a lung apex.
Etiology
This syndrome is often the result of local spread of a tumor of the lung apex, which ends up affecting the chest wall and the base of the neck.
Pancoast syndrome is mainly produced by bronchopulmonary neoplasia, generally nonsmall (adenocarcinoma and squamous), located in the superior pulmonary sulcus or pulmonary apex. However, this syndrome may be due to many other less common causes such as thoracic malignancies or primary or metastatic various infectious causes
Clinical manifestations
Pain in the ulnar aspect of the forearm: It is the earliest symptom and is due to the involvement of the eighth cervical nerve and the first and second thoracic (radicular syndrome involvement of the brachial plexus). Also presents with shoulder pain, braquialgia that typically radiates to the ulnar edge of the arm. There may even be wasting of the muscles of the hand.
Chest pain: Due to destruction of the first and second ribs.
Horner's syndrome : For stellate ganglion sympathetic involvement. It consists of Enophthalmos, ptosis, miosis and facial anhidrosis.
Superior vena cava syndrome: Due to difficulty, compression and invasion, the drainage of the superior vena cava. Depending on the existing collateral circulation, the speed of introduction and the location of the blockage, the clinic will be more or less evident. Characterized by dyspnea, edema of the upper extremity of the body (face, neck and upper limbs), cyanosis and appearance of skin collateral circulation.
The most common presenting symptom is pain shoulder and / or arm ipsilateral to the tumor, as a result of local tumor spread to the parietal pleura, lower brachial plexus, vertebral bodies and the first three ribs. Shoulder pain may radiate to the axilla and the ulnar side of the arm. In most cases the diagnosis is delayed by several months, blending the frame with a painful shoulder syndrome. But besides the shoulder or arm pain may appear associated Horner syndrome, due to involvement of cervical sympathetic system and the lower cervical ganglion.
This syndrome include ptosis, miosis, enophthalmos and sometimes facial anhidrosis all ipsilateral to the tumor.
As you move the picture can produce weakness and atrophy of the intrinsic muscles of the hand. Other symptoms that may occur include dyspnea, coughing, chest pain and even cervical cord compression with onset of paraparesis / paraplegia
Diagnosis
Clinical suspicion of Pancoast syndrome (shoulder pain and / or Horner syndrome) should perform an imaging technique. The first test to be performed is the plain chest radiography in two projections (posteroanterior and lateral), which in most cases evidence the presence of a mass in the lung apex. If before the high clinical suspicion chest x-ray is normal, we must use an imaging technique higher diagnostic yield, such as helical computed tomography (CT) high resolution.
CT allows a better assessment of the local extent of the tumor and the possible presence of mediastinal lymph nodes, vascular involvement, other pulmonary nodules and presence of distant metastases (liver, adrenal, etc.). Therefore, you should always make at least one upper thoracic and abdominal CT.
Magnetic resonance imaging (MRI) provides greater diagnostic yield compared with CT, while MRI is superior to CT in the assessment of the local extent of the tumor (pleural invasion, fat sub pleural, brachial plexus or vascular involvement subclavian) .
More recent is the use of magnetic resonance angiography allows very accurately evaluate the possible vascular involvement of the subclavian vessels and / or brachiocephalic.
The positron emission tomography (PET) is very useful in staging lung neoplasms, especially non-small cell of, since allows a better evaluation of mediastinal lymph node involvement and distant metastases.
Definitive diagnosis requires pathologic demonstration of tumor. Sputum cytology has a low diagnostic yield in these cases, since injuries are treated peripheral location, being diagnostics only 15-20% of cases.
It is often used to bronchoscopy which allows assess the permeability and characteristics of the mucosa of the bronchial tree, with the possible sampling through the bronchial aspirates and / or biopsy / transbronchial needle aspiration of suspicious lesions and lymphadenopathy. Due to the peripheral tumor site often not achieved visualize the tumor, fiberoptic bronchoscopy profitability being 40-60%.
Therefore, the best technique for diagnosis of this tumor is transthoracic needle aspiration.
Other tests include conducting a complete biochemistry with hepatic and renal profile, complete blood count with reticulocyte and peripheral blood smears that may reveal one myelophthisis, in which case they must resort to a biopsy / aspirate bone marrow and performing cranial CT or MRI to rule out brain metastases.
Prognosis and Treatment
Pancoast syndrome by definition occurs at a minimum stage IIB, for Pancoast tumor is a T3 in the TNM classification. The poor prognostic factors Pancoast's syndrome are:
- Weight loss greater than 5%.
- Vertebral involvement.
- Effect vascular or supraclavicular.
- Stage IIIA or higher (N2, N3 or M1).
Survival at 5 years varies depending on the stage of the tumor and for IIB is 45 and 15% for higher stages.
The presence of T4 (tumor of any size that affects the mediastinum, heart, great vessels, trachea, carina, esophagus or vertebral bodies, malignant pleural effusion or separated from the original lung tumor nodules in the same lobe) or lymph node mediastinal N2 (ipsilateral mediastinal lymph nodes or subcarinal) or N3 (bilateral or contralateral mediastinal lymph nodes, supraclavicular or scalene) represent a worse prognosis. Another poor prognostic factor is the presence of distant metastases M1 (stage IV), the central nervous system (CNS) one of the most common sites of distant metastases.
Therefore, before considering the possibility of surgery it is essential to rule out the presence of CNS metastases, by performing cranial CT or MRI.