DEFINITION
Pulmonary Edema Acute Height (EPA), English High Altitude Pulmonary Edema (HAPE) is a non-cardiogenic pulmonary edema that can occur in subjects exposed to hypoxia (decreased oxygen in the blood) due to the height; which affects healthy people.
It comes in heights above 2700 m within the first 4 days after arrival. While it is rare in lower altitudes, they were described in some cases as low as 2000 m heights. It is considered a malignant form of MAM evolving towards resting tachycardia, dyspnea, orthopnea and death.Autopsy studies show injury to the pulmonary capillaries and alveoli occupation by a serous fluid rich in protein.
ETIOPATHOGENESIS
the pathogenesis of the syndrome is unknown, although several theories are invoked:
- Irregular vasoconstriction of the pulmonary vascular bed: With decreased flow in some areas and in other less hyperflow capacity vasoconstriction. Capillaries more afflux trasudarían the socket. This theory does not fully explain why the characteristics of edema are rather exudate transudate.
- Increased pulmonary capillary hydrostatic pressure: With break them and occupation of alveolar macrophages, proteins and red blood cells.
- Retention of water and electrolytes: For activation of the renin-angiotensin-aldosterone system and antidiuretic hormone, and the resulting increase in pulmonary capillary hydrostatic pressure.
The ultrastructural studies by electron microscopy in rats Madison strain, showing a violent pressor response of the pulmonary vascular tree to hypoxia, and simultaneously, are likely to have pulmonary edema, indicates that there is disruption of the capillary endothelium, and even entire vessel structure, with alveolar epithelial edema, and presence of erythrocytes and edema fluid in the wall of the gap.
It is unclear the role of cold air inhaled because, in addition to compromising lung mechanics to cause bronchoconstriction, congestion of airways, increased secretions, and decreased mucociliary clearance, one of the effects of cold air is lower basal ventilation and sensitivity of the chemoreceptors. These responses in animals mean a minimization of heat losses by respiration, but is believed to have great importance in adaptive human. On the contrary, in these, the cold air seems to increase pulmonary vascular resistance, a synergistic response to hypoxia, which can mediate pulmonary hypertension and edema high.
Chronic exposure to cold air may cause hypertrophy of the muscle bundles of the bronchi and increase the thickness of the muscle layers of pulmonary terminal arterioles, which can be an important factor in the appearance of bronchial symptoms of pulmonary arterial hypertension chronic and hypertrophy of the right heart.
The altitude pulmonary edema is the abnormal accumulation of water in the lung due to rupture of the blood-gas barrier lung caused by hypobaric hypoxia. This breakdown develops from a series of responses maladaptive to hypoxia found at higher altitudes, including poor ventilatory response, increased sympathetic, exaggerated tone and uneven pulmonary vasoconstriction (pulmonary hypertension), inadequate oxide production endothelial nitric, and overproduction of endotelina.El end result is an irregular extravascular fluid accumulation in the alveolar spaces that impairs breathing and may, in severe cases, prove fatal.
High mean pressure in pulmonary artery (PA), in excess of 35 to 40 mmHg, appears to be the initiating event. subsegmental specific segmental capillary beds with relatively less vasoconstriction are disproportionately exposed to high pressures microvascular (> 20 mmHg) arising from the pressure of the high average AP. This uneven vasoconstriction and regional overperfusion are a failure of irregular alveolar-capillary barrier and pulmonary edema.
exaggerated pulmonary hypertension
The exaggerated pulmonary hypertension is the fundamental characteristic of HAPE and clearly contributes to its pathogenesis since:
- The HAPE is unfailingly associated with an exaggerated pulmonary hypertension.
- Anatomical abnormalities (congenital absence of the right pulmonary artery, pulmonary arterial occlusion from granulomatous mediastinitis) or functional (Down syndrome) that predispose to pulmonary hypertension they are a risk factor for the development of HAPE at a relatively low height (1,500- 2,500 m).
- The reduction of pulmonary artery pressure with pharmacological agents of different classes has beneficial effects on the HAPE.
- Prevention of pulmonary hypertension in susceptible individuals to HAPE reduces the incidence of pulmonary edema during altitude exposure.
What mode pulmonary hypertension leads to pulmonary edema?
A key step is the transmission of this increase in pulmonary artery pressure into the capillaries. For this to happen, there must be regions where the capillaries are not protected by the contraction of the pulmonary arterioles. This test is effectively what happens in the development of HAPE is that perfusion lung regions with radiological evidence of pulmonary edema is much more marked than in the regions without edema.
Consistent with these findings, we have shown that pulmonary capillary pressure is significantly higher in subjects with HAPE in subjects without that condición30. Finally, a study in which a bronchoalveolar lavage was performed in patients with incipient HAPE, showed the presence of red blood cells and proteins of high molecular weight, findings consistent with pulmonary edema induced shear stress and not by inflammation.
- Mechanisms of pulmonary vasoconstrictor response to exaggerated height susceptible to HAPE subjects.
Role of decreased synthesis and / or pulmonary endothelial nitric oxide bioavailability
Endothelial nitric oxide (NO) plays an important role in regulating pulmonary vascular tone in the human, as their synthesis inhibition by L-NMMA infusion of power generating the vasoconstrictor response in acute hypoxic respiration.
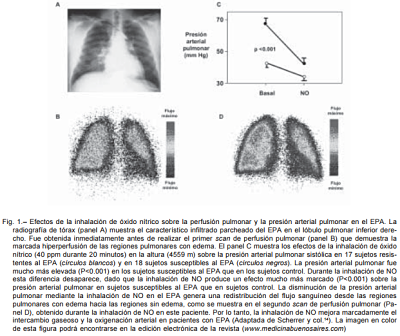
Furthermore, when administered in inhaled, NO attenuates pulmonary vasoconstrictor response generated by exposure to hypoxia. In a recent study, we examined the effects of inhaled NO on pulmonary artery pressure in a group of subjects susceptible to HAPE, and in a group of subjects resistant to this condición14. According to expectations, subjects susceptible to HAPE had a much more pronounced than those resistant to such entity pulmonary vasoconstriction.
During NO inhalation, however, pulmonary arterial pressure was similar in both groups, because the drop in blood pressure induced by NO was much more marked in subjects susceptible to HAPE in resistant. This observation suggests that a defect in the synthesis of NO by the endothelium lung is one of the mechanisms contributing to exaggerated hypoxic pulmonary hypertension in humans. Consistent with these data, seen in some populations of subjects susceptible to HAPE the presence of a polymorphism in the gene encoding the enzyme endothelial nitric oxide synthase (eNOS) generating decreased vascular NO synthesis.Also in other populations characterized by an attenuated pulmonary vasoconstrictor response to hypoxia (and presumably resistance relative HAPE) said polymorphism has been reported associated with increased vascular NO synthesis.
During NO inhalation, however, pulmonary arterial pressure was similar in both groups, because the drop in blood pressure induced by NO was much more marked in subjects susceptible to HAPE in resistant. This observation suggests that a defect in the synthesis of NO by the endothelium lung is one of the mechanisms contributing to exaggerated hypoxic pulmonary hypertension in humans. Consistent with these data, seen in some populations of subjects susceptible to HAPE the presence of a polymorphism in the gene encoding the enzyme endothelial nitric oxide synthase (eNOS) generating decreased vascular NO synthesis.Also in other populations characterized by an attenuated pulmonary vasoconstrictor response to hypoxia (and presumably resistance relative HAPE) said polymorphism has been reported associated with increased vascular NO synthesis.
Role of alveolar epithelial decreased nitric oxide synthesis
In the respiratory system, NO is not only caused by pulmonary vascular endothelium, but also by the respiratory epithelium. There is evidence that the latter also involved in the regulation of pulmonary artery pressure. NO synthesis by the respiratory epithelium, and not the pulmonary endothelial, can be evaluated by measuring NO in exhaled air.
In susceptible to HAPE subjects, acute exposure to hypoxia causes a decrease in the concentration of exhaled. Also, the height, the concentration of exhaled is less susceptible to HAPE than in control subjects (and not increased during the first days of exposure to high) subjects, and therefore there was an inverse relationship between pulmonary artery pressure and the NO concentration.
- High altitude pulmonary edema is interesting to note that at physiological concentrations, NO attenuates oxidative stress, a mechanism has been implicated in the pathogenesis of hypoxic pulmonary hypertension. In situations where there is a deficit in the production of NO, loss of inhibition of oxidative stress represent an additional mechanism to facilitate the development of pulmonary hypertension.
Taken together, these findings indicate that a defect in the synthesis of NO by the endothelium pulmonary and respiratory epithelium contributes to an exaggerated pulmonary hypertension during acute altitude exposure to HAPE in susceptible people.
Role of exaggerated synthesis of endothelin-1
> In addition to vasorelaxant factors, the pulmonary endothelium synthesizes vasoconstrictor factors. The most powerful of them, endothelin-1 (ET-1) plays an important role in the regulation of pulmonary vascular tone during hypoxic stress. In healthy subjects, altitude exposure increases the plasma concentration of ET-1. To examine whether the ET-1 contributes to exaggerated pulmonary vasoconstriction in subjects susceptible to EPA have measured, in a recent study, plasma levels of ET-1 and pulmonary arterial pressure at low altitude (580 m) and height (4559 m) in susceptible and resistant EPA43 subject. At altitude, the plasma levels of ET-1 were significantly higher in subjects susceptible to HAPE in those resistant. We also saw a direct relationship between changes in plasma ET-1 and pulmonary measured between low and high altitude blood pressure.
These findings are consistent with the hypothesis that the increased release of the potent vasoconstrictor peptide ET-1, and / or decreasing their elimination, represents an additional mechanism contributing to exaggerated pulmonary hypertension in height. Finally, and even more interesting is the fact that in human endothelial cells NO inhibits the stimulus for gene expression and synthesis of ET-1 induced by hypoxia, suggesting the presence of a cause-effect relationship between the deficit on NO synthesis and increased synthesis of ET-1.
Role of the sympathetic nervous system hyperactivity
Cardiovascular regulation against hypoxia is mediated, at least in part, by the sympathetic nervous system since it promotes the activation of pulmonary vasoconstriction and fluid accumulation in the alveolar space in experimental animals.
Therefore, it is possible that the sympathetic nervous system may contribute to exaggerated pulmonary hypertension susceptible to HAPE of subjects. To test this hypothesis we measured, in susceptible and resistant to HAPE subjects, sympathetic nerve activity (using intraneural microelectrodes) in skeletal muscle vasculature and pulmonary arterial pressure during altitude exposure. Pulmonary edema in susceptible subjects, activation of the sympathetic nervous system was much more marked. More importantly, this hyperactivity of the sympathetic nervous system precedes the development of pulmonary edema and is directly related to pulmonary arterial pressure.
These data provide the first evidence that subjects susceptible to HAPE have an exaggerated activation of the sympathetic nervous system during altitude exposure, suggesting that it can contribute to exaggerated pulmonary hypertension induced by hypoxia observed in these subjects. Consistent with this hypothesis, it has been shown that subjects suffering from HAPE, infusion adrenergic blocking agent phentolamine alpha generates a much more marked than that nonspecific vasodilators decrease in pulmonary artery pressure. Finally, there is evidence in experimental animals and humans that NO limits the activation of the sympathetic nervous system. It is possible, therefore, susceptible to HAPE in the deficit in the synthesis of NO subjects can contribute to the exaggerated sympathetic activation induced high.
Factors predisposing HAPE
- The factors that predispose this edema are:
- Great physical effort.
- low temperatures.
- High humidity.
- Individual sensitivity to hypoxia.
PULMONARY HIPERTENSSION
exaggerated pulmonary hypertension is the fundamental characteristic of epa. pathologies that can cause pulmonary hypertension (.. sindr Down, absence of pulmonary artery Right, occlusion pulmonary artery by mediastinitis Brushy granule) are risk factors present epa at moderate altitudes (1500 -. 2500 m) lowering medications pulmonary hypertension, epa improve the prevention of pulmonary hypertension in susceptible people, reduce the incidence of epa
MECHANISMS BY WHICH LEADS TO PULMONARY HYPERTENSION EPA
The key mechanism is the transmission of hypertension in the pulmonary artery to the pulmonary capillaries. In patients with epa, it has shown an increase in pulmonary capillary pressure in areas of the lungs with edema.
On the one hand it has been shown that some populations susceptible epa, have less ability to synthesize vascular nitric oxide. (Retail synthesis ons.e. (on endothelial synthetase) Furthermore, relatively resistant patients suffer epa has a increased ability to synthesize vascular nitric oxide (NO).
DEFECTS IN CELLULAR TRANSPORT transepithelial Na +.

- LOW ALTITUDE, THE ELIMINATION OF CELLULAR FLUID is 30% lower in individuals susceptible.
- Suggesting GENETIC DEFECT IN transepithelial transport - HONEYCOMB Na and water.
- PREVENTION OF AN EXCITING THIS ADMINISTRATION OF TRANSPORT a beta adrenergic
- REDUCES THE IMPACT OF PULMONARY EDEMA DURING EXPOSURE TO HEIGHT IN MORE THAN 50%.
Pulmonary edema resulting from an imbalance between the accumulation and removal of fluid airspace. While for many years it has been argued that the forces of Starling and lymphatic system were solely responsible for the drainage of intra-alveolar fluid, it is now known that both active and facilitated, alveolar transepithelial sodium transport also plays an important role. Sodium is taken in the apical part of the alveolar cells, mainly through a channel sensitive to amiloride (ENaC) sodium. After being captured, the sodium is pumped out of the cell by the Na-K-ATPase membrane pump located in the basolateral Water passively follows this osmotic gradient. It is thought that the ENaC represents the limiting step in the alveolar transepithelial sodium transport and water, as deficient in the a subunit of ENaC transgenic rats develop respiratory distress and quickly die after birth due to the inability to reabsorb the fluid from his lungs even more relevant to human pathophysiology, is the fact that when these same rats lacking aENaC are transferred the corresponding gene, they survive to adulthood. However, these rats exhibit substantial decrease in alveolar transport of sodium and water. Under normal conditions, this defect is of no consequence since the alveolar water content is normal. However, under experimental conditions that stimulate the formation of edema, the condition changes dramatically increasing retarding fluid accumulation and disposal. These data demonstrate that a defect in the alveolar transepithelial sodium transport facilitates the formation of pulmonary edema.
EPA CAUSED BY INCREASED PRESSURE CAPILAR
A key step is the transmission of this increase in pulmonary artery pressure into the capillaries. For this to happen, there must be regions where the capillaries are not protected by the contraction of the arterioles pulmonares13. The proof that this is indeed what happens in the development of the EPA is that perfusion lung regions with radiologic evidence of pulmonary edema is much more marked than in regions without edema Consistent with these findings, we demonstrated that capillary pressure lung is considerably higher in subjects with EPA than in subjects without the condition. Finally, a study in which a bronchoalveolar lavage was performed in patients with incipient EPA, showed the presence of red blood cells and proteins of high molecular weight, findings consistent with pulmonary edema induced shear stress and not by inflammation.
clinical presentation
There susceptible to HAPE-resistant subjects HAPE subjects, suggesting the presence of a genetic and / or acquired predisposition, there is no complete resistance. HEPA rarely develops on the first day of altitude exposure but occurs between 36 and 72 hours after arrival at altitude (> 2,500 meters). In contrast, residents of height, pulmonary edema reentry often develops within the first 24 hours after the return to standard.
The beginning is progressive, associated with symptoms of acute mountain sickness: headache, insomnia, anorexia, nausea, vomiting, dizziness, shortness of breath, lassitude, motor incoordination.
Respiratory disorders associated with accentuated gradually progressive dyspnea with cough that is dry and not start with antitussives headquarters due to severe desaturation of blood, if the cough persists hemoptysis appears. Also there is a marked decrease in exercise tolerance, weakness and lethargy. Cyanosis is always present, predominantly at the level of the face and extremities. The pulse is rapid, systemic blood pressure is not always diminished and no ingurgitantes jugular observed. On auscultation of the lungs, and sometimes without auscultation, coarse and fine crackles are perceived.
Electrocardiogram, sinus tachycardia and often high and spiky wave in D2, changes in ventricular repolarization and depolarization is observed reveal a right ventricular overload.

HAPE may be associated with cerebral edema that can dominate the clinical picture and end up in a coma.
transient perinatal hypoxic
Epigenetic predisposing cause hypoxic pulmonary hypertension in humans Adverse events occurring in utero may predispose to cardiovascular and metabolic diseases in adulthood. At birth, a transition between gas exchange by the placenta and gas exchange in the lungs requires changes in the pulmonary blood vessels, which during this period are particularly vulnerable to insults such as hypoxia. In rats, exposure to hypoxia during the first days of life induces a transient increase in pulmonary artery pressure and predisposes to pulmonary vasoconstrictor exaggerated both hypoxia as monocrotaline in adulthood response, there is evidence that this pathological response is mainly related to a functional rather than structural defect. Transient hypoxia during the first days after birth generates a decreased expression of eNOS in the lungs. Therefore, altered synthesis could represent a potential mechanism NO.These findings demonstrate that, in humans, a transient condition of pulmonary circulation during the perinatal period leaves a persistent and potentially fatal imprint, activated in adult life, it predisposes to exaggerated pulmonary hypertension.
BONE SCAN
The radiograph is noticeable, especially at the beginning opacities often located in the middle, parahilar or upper parts of the lung fields can be affected one side but is often at different levels of both lungs opacities are observed.
At initiation of HAPE can be observed linear images corresponding to interstitial edema; in cases seen late and untreated, the images are confluent and cover all lung fields and may be associated with pleural effusion unilateral or bilateral and enlargement of the pulmonary artery and the hilar vessels, cardiac silhouette is unchanged.
The central dilation of the pulmonary arteries is a finding that is observed in almost all subjects after his arrival in height. Therefore, this sign can not be used to predict which individuals will develop an EPA and what will not. Characteristic radiographic features of EPA are patched peripheral infiltrates (less peripheral and central frequency) they may be limited to certain lung fields or be generalized.

No hay comentarios:
Publicar un comentario